Treatment and Diagnostic Streptococcus agalactiae Infection
Folder:
Blog Streptococcus agalactiae morphology culture and cell structure
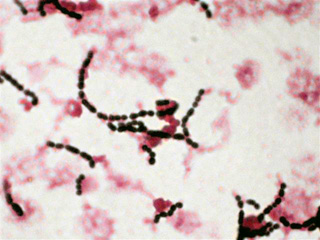
Streptococcus agalactiae belongs to serological group B streptococcal (GBS) due to the antigen characteristics. Morphologically it is gram- positive, round -bearing chains in bacteria. On sheep blood nutrient media containing form around the colonies haemolysis (beta- hemolysis). Hemolysis is but usually less pronounced than that of group A streptococci. Visit: streptococcus-agalactiae.com

Epidemiology
Group B streptococcus (GBS), also known as Streptococcus agalactiae,was once considered a pathogen of only domestic animals, causing
mastitis in cows. Although asymptomatic vaginal carriage of GBS was described in 1935, the first report of GBS sepsis in a neonate was not reported until 1964. Since the 1970s, GBS is recognized as one of the most common causes of neonatal infectious morbidity and mortality in developed countries. GBS causes significant maternal and perinatal morbidity, asymptomatic bacteriuria in pregnancy, and urinary tract and other infections in the adult nonpregnant population. The virulence of S. agalactiae is related to the polysaccharide toxin it produces. Immunity is mediated by antibodies to the capsular polysaccharide and is serotype specific. Several serotypes are known, including Ia, Ib, Ic, II, III, IV, V, VI, VII, and VIII.
Pathogenesis and clinical pictures
S. agalactiae colonizes in the body of some animals, including cow, sheep, and humans without causing any harm. The habitat of this microorganism is largely confined to the intestine and vagina in human and the mammary gland of cows and sheep. This microorganism also colonizes in the genital and/or intestinal tract of about 10-30% of pregnant women.[7] However, some can actually cause diseases in their neonates or immunocompromised mammals. S. agalactiae is the common cause of inflammation or fibrosis of mammary glands and adjacent areas in cows and sheep colonizing the surface of the teat and
duct sinuses. This species causes invasive bacterial infections in mostly neonates and rarely immunocompromised adults, most notably septicemia, neumonia, and meningitis colonizing different locations including the faces, the nose, the umbilical cord, the ears, feces. Infection is spread between cows and/or sheep through the milker's hand, contaminated instrument, and the mouth of calves. Once infected, these mammals are likely to lose their reproductive capacity due to blocked milk channels through inflammation. Infection in humans is through genital and/or intestinal tract of pregnant women either during pregnancy or delivery and from other neonates or members of the hospital staff in the maternity hospital. "The interaction of this bacteria
with host protein and and the entry into host cells thereby represent important virulence traits."
Therapy
The neonatal sepsis due to GBS is because of the serious prognosis of the disease with a combination of penicillin G [(PENICILLIN GRUNENTHAL others) 300,000 IU / kg bw / day in 4-6 divided doses ] or ampicillin [(BINOTAL others) 200 mg / kg bw / day in 3 divided doses ] with an aminoglycoside [eg As gentamicin (Refobacin etc.) ] for at least 5 days treated (pronounced synergism between penicillins and aminoglycosides). Cephalosporins are an alternative to the penicillins. Isolates with reduced susceptibility to b-lactam antibiotics or high levels of resistance to gentamicin come in Germany practically inexistent. The natural sensitivity of B-streptococci to penicillins but by a factor of 10 lower than that of group A streptococci. The percentage of isolates with resistance to erythromycin (Erythrocin, etc.) in all group B streptococci is given as approximately 10%.
In the detection of a B streptococcal colonization between the 35th and 37th week of pregnancy is suggested chemoprophylaxis at the time of birth. In question penicillin G are (initially 5 million IU iv and then 2.5 million IU iv every 4 hours until delivery) or ampicillin (2 g IV at the beginning and then 1 g IV every 4 hours until delivery). In penicillin allergy can clindamycin [(Sobelin others) 900 mg iv ] every 8 hours - not expressly approved in Germany with this indication) or erythromycin (500 mg administered intravenously every 6 hours) until delivery. With the use of erythromycin (about 10% in this country) should previously a sensitivity test can be performed to prevent a failure of prophylaxis of infection due to the resistance situation.